Oral health affects whole body health. Your mouth is the gateway to the rest of your body and how you treat your teeth and gums can have lasting effects.
The brightest of smiles are surrounded by invisible bacteria. With a healthy immune system and excellent oral hygiene, these bacteria are mostly rinsed away…until the next meal.
Practicing daily oral hygiene at home, and partnering with your dentist keeps your body healthier. But, poor oral care leads to gums that recede, called periodontal (gum) disease, which then allows the microscopic bacteria to travel throughout your body.
Leading Researchers Agree
All of these research institutions share the viewpoint that oral health is an essential part of staying healthy. And it goes both ways – bad oral health can cause medical problems, and certain medical problems and medications can contribute to periodontal disease and tooth bone loss.

What We Know Now
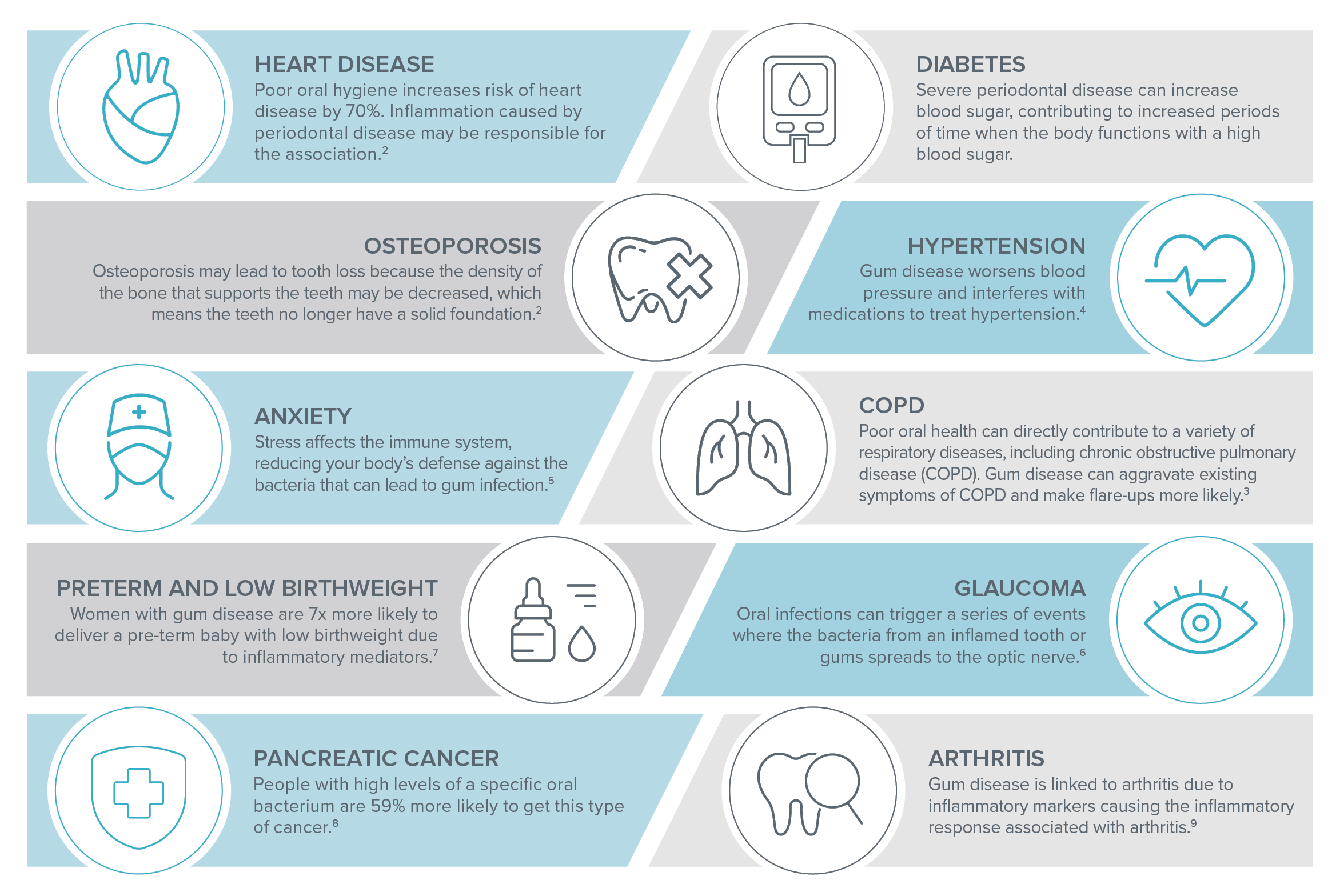
Latest research shows that the primary association between oral health disease and systemic health lies in chronic inflammation and bacteria affecting and entering the bloodstream through the mouth. Inflammatory markers in the bloodstream affect immune response and pathogenic bacteria in the bloodstream can be passed to the whole body.1
What We Do For Our Patients
At each appointment, Willamette Dental Group providers review risk factors for tooth decay and gum disease, including tobacco use and chronic diseases. As a result of this assessment, patients receive a personalized and detailed Proactive Dental Care Plan with recommendations for home care as well as in-office treatments. Additionally, all patients undergo blood pressure checks prior to procedures and are screened for oral cancers. Tobacco users also receive tobacco cessation counseling.
Linking Systemic Disease to Oral Disease
References
2. Penn Medicine and Centers for Disease Control and Prevention. https://www.pennmedicine.org/updates/blogs/heart-and-vascular-blog/2019/march/gum-disease-and-heart-disease
3. Sharma, N. and Shamsuddin, H. (2011), Association Between Respiratory Disease in Hospitalized Patients and Periodontal Disease: A Cross-Sectional Study. Journal of Periodontology, 82: 1155-1160. doi:10.1902/jop.2011.100582
4. AHA Journal (2018), Poor Oral Health and Blood Pressure Control Among US Hypertensive Adults, Hypertension. 2018;72:1365–1373
5. Solis AC, Lotufo RF, Pannuti CM, Brunheiro EC, Marques AH, Lotufo-Neto F. Association of periodontal disease to anxiety and depression symptoms, and psychosocial stress factors. J Clin Periodontol. 2004;31(8):633-638. doi:10.1111/j.1600-051X.2004.00538.x
6. American Academy of Ophthalmology (2016), https://www.aao.org/eyenet/article/oral-health-poag
7. Haerian-Ardakani, A., Eslami, Z., Rashidi-Meibodi, F., Haerian, A., Dallalnejad, P., Shekari, M., Moein Taghavi, A., & Akbari, S. (2013). Relationship between maternal periodontal disease and low birth weight babies. Iranian journal of reproductive medicine, 11(8), 625–630.
8. Harvard Medical School, https://www.health.harvard.edu/staying-healthy/gum-disease-may-signal-warning-for-pancreatic-cancer
9. Bingham, C. O., 3rd, & Moni, M. (2013). Periodontal disease and rheumatoid arthritis: the evidence accumulates for complex pathobiologic interactions. Current opinion in rheumatology, 25(3), 345–353. https://doi.org/10.1097/BOR.0b013e32835fb8ec
10. National Institute of Dental and Craniofacial Research, https://www.nidcr.nih.gov/health-info/hiv-aids